New Parents? New Aches! Looking After Your Body While Looking After Your Kids (& Grandkids)
As a father of two young boys (aged 3 and 1), I know how physical parenting can be. Lifting toddlers, carrying strollers, changing diapers, and spending lots of time on the floor all add up. Most parents expect to be tired — fewer expect the aches and pains that come with it.
Caring for young children often puts our bodies into a flexed posture: rounded shoulders, tight hips, and a sore lower back. When this becomes your daily norm, pain can creep in.
Common Aches New Parents Experience & How to Stretch & Strengthen
Lower back pain
Cause: Frequent lifting and bending
Stretch: Child’s pose — kneel on the floor, sit back on your heels, reach arms forward. Hold 20–30 seconds.
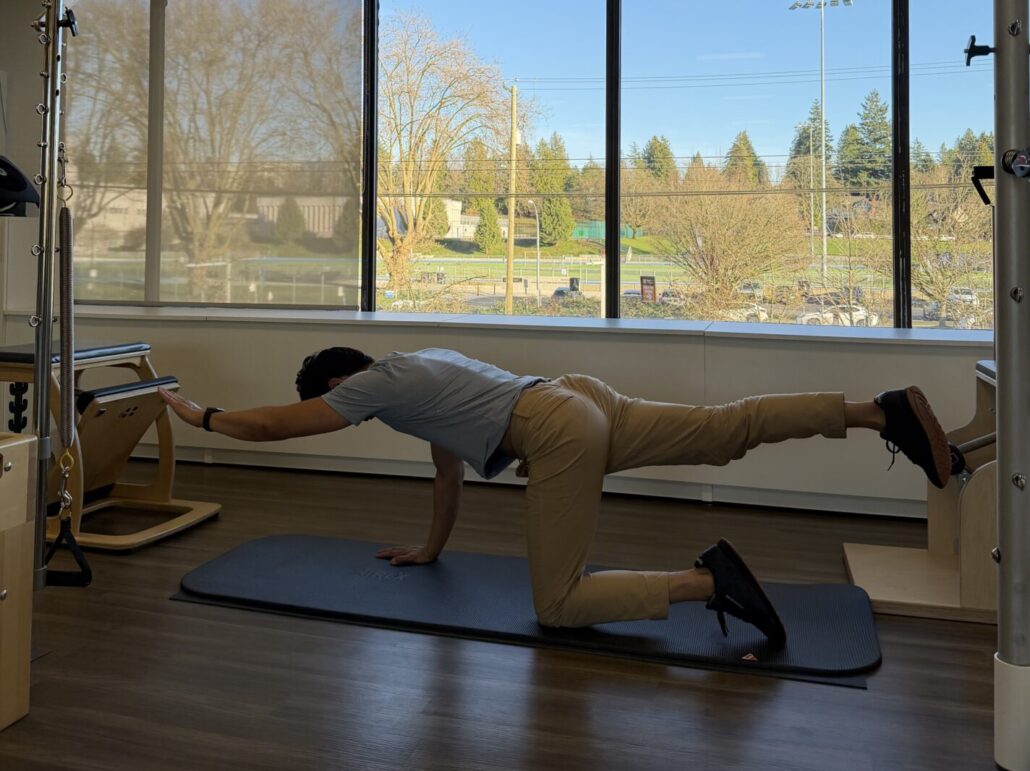
Strengthening: Bird-dog — on hands and knees, extend opposite arm and leg, keeping core engaged. Hold 5–10 seconds, repeat 5–10 times per side.
Neck and shoulder tension
Cause: Feeding, rocking, and carrying
Stretch: Upper trapezius stretch — gently tilt ear toward shoulder, assist with hand, hold 20 seconds each side.
Strengthening: Scapular squeezes — sit or stand tall, squeeze shoulder blades together, hold 5 seconds, repeat 10–15 times.
Wrist or thumb pain (“Mommy’s thumb” / De Quervain’s)
Cause: Repetitive lifting and gripping, particularly lifting from under a toddler’s arms.
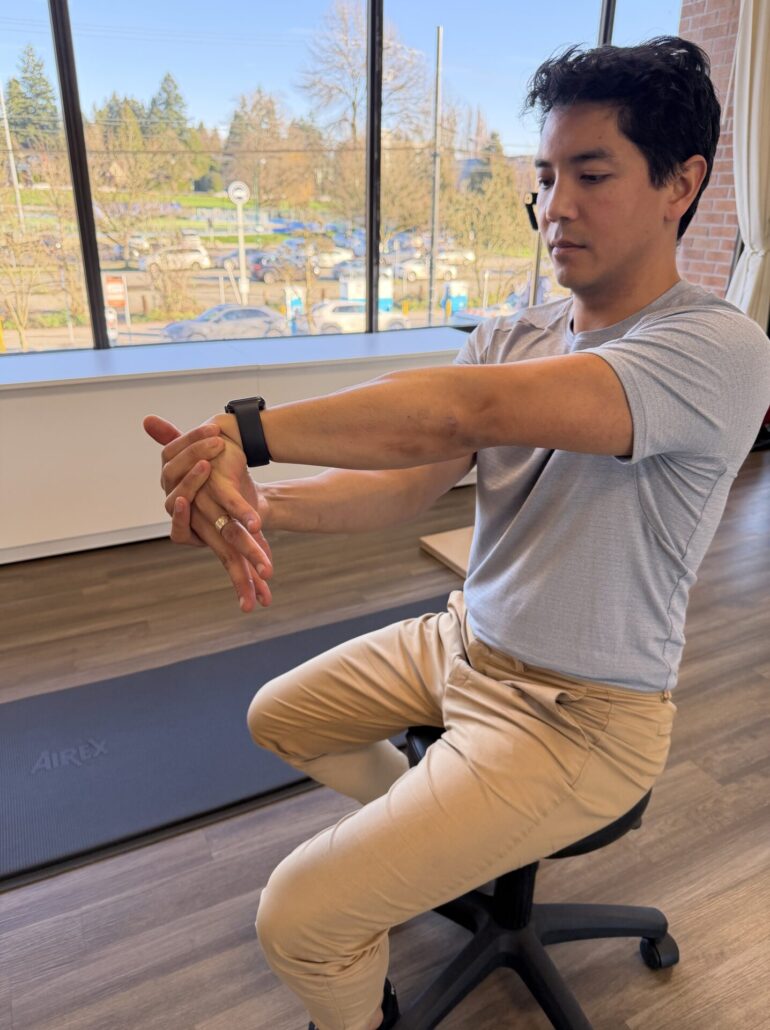
Stretch: Thumb and wrist stretch — gently place thumb inside a loose fist, and tilt the wrist away from your thumb. Hold 30 seconds.
Strengthening (after an initial period of rest and/or bracing): Thumb extension — use a light resistance band around thumb and fingers. Slowly move thumb away from the fingers against resistance. Repeat 10 times.
Forearm pain near the elbow
Cause: Sustained hold of baby
Stretch: Elbow extension. Extend elbow and pronate the forearm, and flex your wrist using your other hand. Hold for 30 seconds.
Strengthening: In this scenario, the stretching is often more important as you are building isometric strength while holding your baby!
Hip tightness
Cause: Prolonged sitting or floor time
Stretch: Half-kneeling hip flexor stretch — one knee on the floor, other foot forward, gently shift weight forward, core engaged. Hold 20–30 seconds each side.
Strengthening: Glute bridges — lie on your back, knees bent, lift hips off the floor, hold 2–3 seconds, repeat 10–15 times.
Finding Time When There Is No Time
For most parents, finding extra time to exercise feels unrealistic. If this is the case, instead of adding something new to your day, I suggest to move with your kids. Toddlers love crawling, climbing, and playing — and many of these movements are exactly what our bodies need.
Play that helps your body too:
- Crab walk: Opens the chest and strengthens shoulders, countering rounded posture.
- Bear or lizard crawl: Builds core, shoulder, and hip strength while staying mobile.
- Stretching during playtime: Use a half-kneeling position to stretch hip flexors while keeping your core engaged while staying at eye level height with your kids.
Even short bursts of play like this help reverse the hunched posture parents often develop. Physiotherapy can help you stay comfortable, confident, and able to keep up with your kids — now and as they grow!